Aesthetic Training Academy directors Drs Simon & Emma Ravichandran discuss the art of the consultation and share two case studies with Aesthetics Journal on behalf of Merz Aesthetics.
Merz Innovation Partners Dr Emma Ravichandran and Dr Simon Ravichandran discuss the consultation and share two different patient journeys
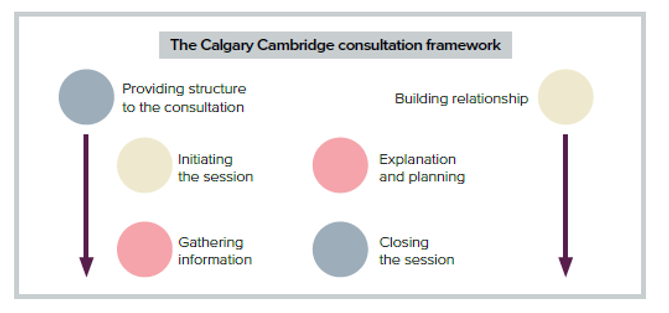
Consultation and communication skills are frequently undervalued. In private practice, our livelihoods are dependent on patient satisfaction, so we need to enhance the patient journey. There are six components to consultation – based on the Calgary Cambridge consultation framework1 – with two overarching pillars
- Building the relationship
- Providing structure to the consultation
- The patient journey can be broken down further into four parts:
- Initiating the session
- Gathering of information
- Explanation and planning
- Closing the session
An effective consultation means effective communication, and that means recognising that individual patients require individual approaches and adapting your processes accordingly.
Over the past 14 years Drs Simon and Emma Ravichandran have created a blueprint for the Clinetix consultation, which combines the Calgary Cambridge framework with a check-in/check-out process adapted from airlines.
Initiating the session
Before the patient even walks into the room, be organised and prepared. Clear the notes from your previous patient and clear your mind. Go out and call the patient in yourself and guide them into the room. This breaks down that barrier of having to walk into a clinical room, which can create anxiety. If a member of your team brings them in, stand up and welcome them. Be aware of your body language. Be comfortable and confident and, most importantly, smile.
Gather information
The amount of information you can get out of a patient in just a few seconds is phenomenal. It only takes six seconds to identify non-verbal behaviours indicative of a personality trait, so think about what they are telling you with their words, body language and non-verbal cues. What are their motivations for treatment?
It is also really good to think about the interaction from your point of view. What feeling do you get from this person? Do you want to treat them? When you develop relationships with your long-term patients, it is a two-way process. As humans, we often mimic other people’s body language. So if someone walks in and is laid back and relaxed, then instantly, the other person is more comfortable. If a patient walks in and has very closed body language, the natural human instinct is to mimic that body language. One of you needs to be the open one, and it has to be you.
When you are gathering your information, you need to:
- Establish eye contact: let the patient know you are listening.
- Encourage specificity: get details about the big picture as well as the small picture.
- Summarise information: recap, check for and correct misunderstandings and miscommunication.
- Practice active listening: respond to visual and verbal cues about distress and explore them further.
- Avoid interruption: studies have shown doctors interrupt their patient after less than 15 seconds
There are several ways in which a patient can derail the consultation, which are discussed below.
Explanation and planning
Use patient photographs as educational tools to describe how the treatments you are proposing may deliver the results the patient is seeking. You can also do this by using a mirror and physically lifting tissues or pointing to the patient’s face. Always ask for permission before touching a patient’s face. Once you have decided on a treatment plan, you can discuss the time frame, the downtime, which treatment you would do first and the intervals between treatments.
Closing the session
The closing of the session is where patients are often lost. The patient has got to be free to decide for themselves, with no pressure, and they should be given time to do that, but they might need guidance on the next steps.
Offer them options such as:
- If you are ready to book, I can book that in now. We can create your treatment plan and get everything organised.
- If you are not ready to book and you decide this is not for you, that’s ok. If you ever want to come back and speak to me, just get in touch.
- If you need more time, time is good. People who rush into decisions are much more likely to regret the outcomes. What information do you need to help you make a decision?
Don’t just shake their hand and let them go out. Instead, walk them to the door. They have got to have that luxury feel, that emotional engagement. We introduce the patient and the next steps to our receptionist and have a conversation while any transactions occur. Then we take them to the door. If they need a taxi, we order them a taxi. When they leave the clinic, we want them to feel like they have just walked out of Louis Vuitton with a handbag. Every patient then gets an email to summarise the consultation, regardless of whether they have booked or not.
The key is to do everything possible to make them feel that this is the best customer service experience they will have. If they say ‘no’, respect that. They will still tell someone else they have had the most informative meeting with the doctor they have ever had.
Case Studies
Simon’s patient – Georgia
Georgia is a patient in her early 30s. She is a performer and works in the public eye in front of cameras.
“The information I have on a patient the first time I see them can be a little or a lot. In Georgia’s case, I knew her age and the fact she was a performer,” says Dr Simon Ravichandran, “So, we know straight away that we have to approach her in a certain way.”
He continues, “You may have your own pre-conceived ideas of what patients in this age group want, and this is the first mistake. You have to wipe that slate clean and approach every patient with a completely open mind. In Georgia’s words, she wanted to ‘feel confident’ and ‘good in her own skin’. We have questioned thousands of patients to find out their motivations for treatment and every time the most powerful motivator is confidence.”
He concludes, “Whenever we see Georgia, she is very smiley and positive, her body language is open, she seems very comfortable in the clinic, so you want to be part of her success story.”
Emma’s patient – Jac
Jac is a 50-year-old patient. She has raised three children on her own for the last 12 years while working full time, but has commented that she doesn’t recognise herself in the mirror anymore.
“When Jac came in, she had a slightly sad demeanour,” explains Dr Emma Ravichandran, “Whenever she is talking about her motivations for treatment, she seems as if she has really thought about and processed these thoughts. She has had some tough times in the past and seems less comfortable than Georgia did but, on the other hand, she still has very open body language and is a very likeable person. You feel a genuine warmness towards Jac and want to help her achieve her goal to be the person she feels inside.”
Dr Ravichandran adds, “She told us she looked in the mirror and said, ‘who is that looking back at me?’ That’s a huge motivator for patients and something we can really help them with, which is a huge privilege.”